There is a whole load of ultrasound images added to my site at:
http://www.ultrasound-images.com/ The site has been pepped up with a new look and easy to use interface. I have added a search box on the home page to sift through the contents of the site. I wanted to add a slide show option for the images but found it problematic. As before, all images are free to view.
1) At the page: http://www.ultrasound-images.com/fetus-general.htm is a case of IUFD with Spalding’s sign. Many books these days simply don’t have images of this sign.
2) At http://www.ultrasound-images.com/early-pregnancy.htm , there is nice case of bicornuate uterus with a gestation sac in one cornu.
3) At http://www.ultrasound-images.com/fetal-brain.htm : I have added a rare image of Vein of Galen aneurysm.
4) At: http://www.ultrasound-images.com/fetal-heart.htm : there are new cases of fetal cardiac anomalies including AVSD and pericardial mass. I hope to add some nice fetal echo videos to this section, but need a little help to edit mpg videos. Can somebody help me?
There are plenty more pictures but, I’ll tell you later.
JOE ANTONY, MD.
Wednesday, November 21, 2007
Thursday, October 04, 2007
Announcing my new ultrasound images website:
Hi all,
After having observed the runaway success of my older site (the ultrasound gallery) at: http://drjoea.googlepages.com/ I have now shifted the action to my new 200 GB capacity site at:
http://www.ultrasound-images.com/ The main features of the new web site is:
1) plenty of byte space.. you can expect loads of free high resolution sonographic images here, plus ultrasound videos when I get them.
2) More bandwidth for web access.
3) Faster download times
I have added a couple of cases already. See:
a) http://www.ultrasound-images.com/fetal-brain.htm where I discuss a fetal anomaly, Dandy-Walker malformation.
b) http://www.ultrasound-images.com/musculoskeletal.htm where I have a case of Medial Cruciate ligament injury.
Dr.Joe Antony, MD.
After having observed the runaway success of my older site (the ultrasound gallery) at: http://drjoea.googlepages.com/ I have now shifted the action to my new 200 GB capacity site at:
http://www.ultrasound-images.com/ The main features of the new web site is:
1) plenty of byte space.. you can expect loads of free high resolution sonographic images here, plus ultrasound videos when I get them.
2) More bandwidth for web access.
3) Faster download times
I have added a couple of cases already. See:
a) http://www.ultrasound-images.com/fetal-brain.htm where I discuss a fetal anomaly, Dandy-Walker malformation.
b) http://www.ultrasound-images.com/musculoskeletal.htm where I have a case of Medial Cruciate ligament injury.
Dr.Joe Antony, MD.
Wednesday, September 19, 2007
Viral fever epidemic in Kerala
Kerala is once again in the grip of a viral fever. This time the situation is worse than last year (2006). All the more mysterious is the fact that most lab tests are negative for most known pathogens (viruses) and the cause is presumed to be chikungunya virus. Then why are tests for chikungunya negative. Possibly, this time (May to Sep 2007), the virus is a mutated sub-strain. Worst is the distribution of the epidemic; whole villages and towns in the rural areas are affected, sparing almost no one. Surprisingly, children are relatively spared with the elderly worst affected. As before, most patients have symptoms of severe bodyache, low grade fever and joint pain and swelling.
Treatment:
1) bed rest
2) Meftal 500 mg (oral) -2 to 3 times a day is found to be VERY effective in controlling the joint pain and bodyache. (Meftal- is mefenamic acid with paracetamol). Caution: not be taken on empty stomach. May cause gastritis.
3) plenty of fluids
Note: Please consult your physician before starting treatment.
Treatment:
1) bed rest
2) Meftal 500 mg (oral) -2 to 3 times a day is found to be VERY effective in controlling the joint pain and bodyache. (Meftal- is mefenamic acid with paracetamol). Caution: not be taken on empty stomach. May cause gastritis.
3) plenty of fluids
Note: Please consult your physician before starting treatment.
Tuesday, September 18, 2007
18th September- update
Have a look at some of the best 3D images of Cleft palate (with cleft lip) available on the internet at: http://drjoea.googlepages.com/obstetric-3 This is 3D sonography at its best. Also added to the free gallery: a new page on lesions of the pancreas at: http://drjoea.googlepages.com/pancreas The first case here is one on pancreatitis.
Dr. Joe Antony, MD
Dr. Joe Antony, MD
Thursday, September 13, 2007
Update- 13th september 2007
At the link: http://drjoea.googlepages.com/nice-pictures
I have added a few images of a nice case of a hypertrophied clitoris in a female fetus. Also, an amusing picture of fetal activity..(check it out).
I have added a few images of a nice case of a hypertrophied clitoris in a female fetus. Also, an amusing picture of fetal activity..(check it out).
Tuesday, September 11, 2007
Update for 11th september 2007:

At the link: http://drjoea.googlepages.com/nice-pictures I have created a new page on my free ultrasound gallery that deals with interesting, amusing and insightful sonographic images. Enjoy..and good scanning to all fellow imagers.
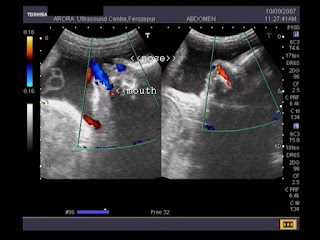
And, here are some nice pictures from Dr. Vikas Arora, India. They show that the fetus often aspirates and regurgitates fluid from the nose and mouth.
And, here are some nice pictures from Dr. Vikas Arora, India. They show that the fetus often aspirates and regurgitates fluid from the nose and mouth.
Ultrasound images large varicocele
Sunday, September 09, 2007
Updates for 9th September 2007:
Check: http://drjoea.googlepages.com/musculoskeletal for ultrasound images of Achilles tendonitis.
Also have a look at the images posted at:
http://drjoea.googlepages.com/obstetric-3 where I present a case of fetal abdominal cyst.
As usual, you'll find free high resolution images.
Dr. Joe Antony, MD.
Also have a look at the images posted at:
http://drjoea.googlepages.com/obstetric-3 where I present a case of fetal abdominal cyst.
As usual, you'll find free high resolution images.
Dr. Joe Antony, MD.
Tuesday, September 04, 2007
Sonography of deep vein thrombosis:
Check out some lovely and self-explanatory, color doppler and gray-scale ultrasound images of Deep vein thrombosis at: http://drjoea.googlepages.com/vascular These images are well labelled and of the highest resolution. The added text describes the various techniques used to diagnose thrombosis.
Dr. Joe Antony, MD.
Dr. Joe Antony, MD.
Saturday, September 01, 2007
New additions to my free online gallery of ultrasound images:
The past week has been hectic. I have added a number of 3-D sonographic images to my web site at:
http://drjoea.googlepages.com/obstetric-3 For the lay person, there are a number of lovely 3-D images of the fetus in various moods. For the sonologist and sonographer, there are images of cystic lesions of the umbilical cord, anenecephaly and macroglossia.
At: http://drjoea.googlepages.com/uterus-2 , I discuss a case of hematometrocolpos.
If you have any interesting sonography related cases or queries, do write to me at :
drjoea@gmail.com
Dr.Joe Antony, MD.
Cochin, India.
http://drjoea.googlepages.com/obstetric-3 For the lay person, there are a number of lovely 3-D images of the fetus in various moods. For the sonologist and sonographer, there are images of cystic lesions of the umbilical cord, anenecephaly and macroglossia.
At: http://drjoea.googlepages.com/uterus-2 , I discuss a case of hematometrocolpos.
If you have any interesting sonography related cases or queries, do write to me at :
drjoea@gmail.com
Dr.Joe Antony, MD.
Cochin, India.
Monday, August 20, 2007
A Vesico-ureteric junction calculus:
Thursday, August 16, 2007
A different sonographic approach to pick up ureteric calculi:

This is an ultrasound image of a distal ureteric calculus. What makes it so special is that it was diagnosed by transvaginal scan. Dr. Gunjan Puri, MD, Surat, India finds this approach, helps detect ureteric calculi which are difficult to pick up by transabdominal scan. Color doppler helps confirm the diagnosis with the typical twinkling sign.
You can see more such ultrasound images of the urinary tract at:http://drjoea.googlepages.com/urinarytract
You can see more such ultrasound images of the urinary tract at:http://drjoea.googlepages.com/urinarytract
Saturday, July 21, 2007
The mystery of the periprostatic vessels:
Whilst doing a TRUS (Transrectal Ultrasound scan) for the prostate, seminal vesicles, etc., I have often come across these large, anechoic, tubular structures (V) on either side of the lateral lobes of the prostate. After reading extensively on the topic, I have found few answers. In this transverse section, the tubes (V) are seen well.
Note the inhomogenous echotexture of the prostate, with some hyperechoic area in the left side of the inner gland s/o chronic prostatitis. The patient was a young man with history of chronic dysuria and lower abdominal pain.


On sagittal section, the structures can be traced anteriorly and inferiorly.. definitely not the ureters.

Oblique transverse sections show the vessels communicating with their counterpart from the other side. Obviously these are vessels, most likely to be the periprostatic venous plexus.
Note the inhomogenous echotexture of the prostate, with some hyperechoic area in the left side of the inner gland s/o chronic prostatitis. The patient was a young man with history of chronic dysuria and lower abdominal pain.


On sagittal section, the structures can be traced anteriorly and inferiorly.. definitely not the ureters.

Oblique transverse sections show the vessels communicating with their counterpart from the other side. Obviously these are vessels, most likely to be the periprostatic venous plexus.
Diagnosis: prostatitis with dilatated periprostatic veins.
Saturday, July 07, 2007
Sonography of bilateral renal agenesis in a fetus:


 This is yet another case of bilateral renal agenesis.
This is yet another case of bilateral renal agenesis.This case is presented by Dr. Ajit Athale, MD, from Baroda, India. He describes the findings nicely. These images are of a fetus of 28 weeks.
Here we can see the "LYING DOWN" ADRENAL SIGN, the diagnostic finding ofof renal agenesis. In renal agenesis, the adrenals are free to occupy the space left in the renal fossa. So instead of being horizontal & being contoured frombelow by the upper pole of kidneys, they become vertical and flat, literally, plate like. This flattening of the adrenals is an indirect sign that the kidneys did not develop in the flanks. In fact, even on postmortem, I (Dr. Ajit) have seen pathologists mistaking gross specimen of discoid shaped adrenals as kidneys in case of bilateral renalagenesis, only to be corrected later on- by microscopy.This sign is of particular importance when one is notsure as to presence or absence of kidneys.Sometimes domes of diaphragm can masquerade as upperpoles of kidneys, especially when fetus is breathing (as shown in one of my pictures).This fetus also had club foot.
For more on this topic and view some more ultrasound images of renal agenesis, please visit my gallery of ultrasound images at:
http://drjoea.googlepages.com/obstetric-2
http://drjoea.googlepages.com/obstetric-2
Tuesday, June 12, 2007
Saturday, April 21, 2007
The case for sonohysterography:


For some time, sonohysterography was considered essential to diagnose endometrial polyps. Until, high resolution ultrasound and endovaginal probes challenged that assumption with stunning images on routine ultrasound scan. These images by Dr. Allen Worrall, Alaska, USA, show an instance, wherein, sonohysterography may well be advisable, to confirm the presence of a doubtful polyp
Wednesday, April 04, 2007
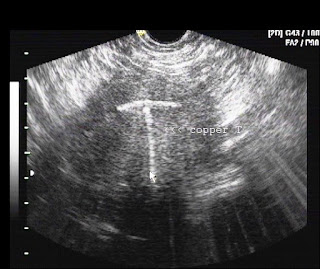
A comparison of sonographic features of intrauterine contraceptive devices (IUCD’s):

The Mirena IUCD
Mirena IUCD used in USA
Copper - T, IUCD
Dr. Allen Worrall, of Fairbanks Clinic, Alaska, USA has this to say about IUCD or IUDs:
The hormone-containing Mirena IUCD is quite popular in the US now. It has a somewhat different sonographic signature than other IUCDs. (in the US, IUD mostly stands for IntraUterine Device). The presence and location of the Mirena IUCD is mostly from its acoustic shadow - you tend not to see the actual echo of the device very well.
This case is interesting because as I (Dr. Allen) scanned the uterus transversely, starting at the cervix, I could see the string as a bright echo with hardly any shadow, then suddenly there was no echo but an intense shadow, representing the shaft of the IUCD. The Mirena has two curved arms at the top that are supposed to extend out when the IUCD is properly positioned. On transverse view of the upper part of the uterus I could see that the arms were properly deployed.
This patient had this IUCD or IUD only for a few weeks and was complaining of cramps and bleeding. The doctor who put the IUD in wanted to be sure it was in proper position. I reported that it was OK.
This IUD was put in place because the patient was complaining of excessively heavy menses, and the Mirena IUD, because of its hormone content often results is less bleeding. Interesting to me, who can remember when IUDs had the reputation of causing abnormal, excessive, prolonged bleeding. Now they are used to treat those symptoms.
Images courtesy of Dr. Allen Worrall and Dr. Joe Antony.
The hormone-containing Mirena IUCD is quite popular in the US now. It has a somewhat different sonographic signature than other IUCDs. (in the US, IUD mostly stands for IntraUterine Device). The presence and location of the Mirena IUCD is mostly from its acoustic shadow - you tend not to see the actual echo of the device very well.
This case is interesting because as I (Dr. Allen) scanned the uterus transversely, starting at the cervix, I could see the string as a bright echo with hardly any shadow, then suddenly there was no echo but an intense shadow, representing the shaft of the IUCD. The Mirena has two curved arms at the top that are supposed to extend out when the IUCD is properly positioned. On transverse view of the upper part of the uterus I could see that the arms were properly deployed.
This patient had this IUCD or IUD only for a few weeks and was complaining of cramps and bleeding. The doctor who put the IUD in wanted to be sure it was in proper position. I reported that it was OK.
This IUD was put in place because the patient was complaining of excessively heavy menses, and the Mirena IUD, because of its hormone content often results is less bleeding. Interesting to me, who can remember when IUDs had the reputation of causing abnormal, excessive, prolonged bleeding. Now they are used to treat those symptoms.
Images courtesy of Dr. Allen Worrall and Dr. Joe Antony.
Wednesday, March 14, 2007
The case of the knotty cord:

 The umbilical cord connects the placenta (and thus the mother) to the baby. Occassionally, the cord can get knotted, presenting a real danger to the baby, by strangulation of its lifeline. We present a case of knot of the cord, diagnosed prenatally by color doppler imaging. The post delivery snaps confirm the presence of true knot of the cord. Images courtesy of Dr. Gidda Ramaiah, India. Check this link for pics and description: http://drjoea.googlepages.com/obstetric-2
The umbilical cord connects the placenta (and thus the mother) to the baby. Occassionally, the cord can get knotted, presenting a real danger to the baby, by strangulation of its lifeline. We present a case of knot of the cord, diagnosed prenatally by color doppler imaging. The post delivery snaps confirm the presence of true knot of the cord. Images courtesy of Dr. Gidda Ramaiah, India. Check this link for pics and description: http://drjoea.googlepages.com/obstetric-2
On the importance of first trimester sonography:
Dr. Allen Worrall of Alaska, USA, has this to say about the role of the early first trimesterultrasound scan. The First ultrasound always sets the gestational age. Subsequent ultrasounds determine the growth of the baby. You never change a due date based on a second or third ultrasound (assuming in all cases of course that the first ultrasound was done correctly, by someone who knows what they are doing, and using a machine that accurately makes the measurements).
Why is the first ultrasound always the most accurate in determining gestational age? Because we use the size of the baby to determine gestational age, and we do not all weigh exactly the same at birth. The closer we get to term, the more our "genetic heritage" is manifesting itself to make us small, average, or large. Or to put it another way: at around 8-10 weeks gestation we all are about the same size for a given gestational age. At 34-36 weeks gestation some of us are going to be small for our gestational age, some of us are going to be just about the size expected for our gestational age, and some of us are going to be large for our gestational age.
Mean Sac Diameter (MSD) is not as accurate as CRL. MSD is best used at very early gestational age when all you can see is the yolk sac, perhaps a heart beat, but you really cannot see the embryo yet. We are talking about 5w and a few days, by high resolution transvaginal scan.
From me: that was beautiful; you could not have put it better.
Why is the first ultrasound always the most accurate in determining gestational age? Because we use the size of the baby to determine gestational age, and we do not all weigh exactly the same at birth. The closer we get to term, the more our "genetic heritage" is manifesting itself to make us small, average, or large. Or to put it another way: at around 8-10 weeks gestation we all are about the same size for a given gestational age. At 34-36 weeks gestation some of us are going to be small for our gestational age, some of us are going to be just about the size expected for our gestational age, and some of us are going to be large for our gestational age.
Mean Sac Diameter (MSD) is not as accurate as CRL. MSD is best used at very early gestational age when all you can see is the yolk sac, perhaps a heart beat, but you really cannot see the embryo yet. We are talking about 5w and a few days, by high resolution transvaginal scan.
From me: that was beautiful; you could not have put it better.
Tuesday, February 13, 2007
Radiology grand rounds IX on Cochinblogs:
10 ways to limit your liability on call, in no particular order: by Mikhail Serebrennik
(quoted from http://www.filmjacket.com/news.php?readmore=54 with permission)
The most important thing is to escape responsibility or at least spread it among as many people as possible, so that you are never solely responsible for a suboptimal outcome. Here are 10 ways to do it.
Disclaimer: Of course, everything in this article is for entertainment purposes only; you should use sound medical judgment, reliable information sources and practice guidelines accepted at your institution at all times, and do everything in the best interest of patient care.
1. Request additional and/or short-term follow-up studies - if you don't know what the heck you are looking at, this may result in someone else having to read the additional/follow-up studies and carry a part of the burden of final decision.
2. Talk to the referring clinician - they may point you in the right direction and even give you the differential diagnosis. Armed with a decent differential, you may be able to produce a reasonable report.
3. Suggest clinical correlation. This is self-explanatory.
4. Call and wake up your attending - it's better to annoy them now than surprise them the next day. If your attending tells you to buzz off and hangs up on you, you've done your part - the responsibility has been spread.
You can read the rest of this piece at: http://www.filmjacket.com/news.php?readmore=54


Dr. Sumer Sethi and Dr. Joe Antony invite case submissions for the next radiology grand rounds IX on cochinblogs. The cases and/ or articles related to radiology will be put on 25th Feb 2007. Anybody interested in radiology including sonography,
conventional radiology, CT scan, MRI etc. may submit their articles, cases etc. to drjoea@gmail.com .
Here is an interesting case.
A 32 yr old comes with history of non specific pain in the knee joint.
Clinically he is normal.
MRI shows a well defined a focal altered signal intensity lesion seen in close proximity to Post cruciate ligament . It is to be differentiated from PCL tear.
Diagnosis: Posterior cruciate ligament ganglion.
Brief description of Posterior cruciate ligament
· Prevents post displacement of tibia on femur
· Extends from med femoral condyle to post and inf to tibial articular surface
· Average length 38 mm and width midpart 13 mm
· Like ACL is intraarticular and extrasynovial
· Vascular supply from middle genicular artery of popliteal vessel
· Ganglion may attach to PCL
· It is differentiated from PCL tear by demonstrating intact underlying PCL and well defined nature of ganglion.
Case presented by Dr. MGK Murthy.
Dont forget to visit our sister site: the free gallery of ultrasound images
Here you'll find loads of interesting sonographic images with a brief description and the best reference links.
A hole in the ….? A case by Dr. G.C. George (http://med97um.net/george/ )

Many have heard of a hole in the heart but for this 58 year old gentleman, it was a totally different story. He was assisted into ER, wailing in pain with every single movement. It was all too sudden. Even taking a deep breath was difficult as the pain was excruciating. He was sweating, his pulse racing, he could barely speak because the slightest effort caused him intense pain.The pain occured suddenly, all over the abdomen causing it to be so “board -like” He could barely move. He requested to be propped up to allow him to breath easily. He never had any such pain before but recently was taking some herbal traditional medication for better health! Yeah sure! My medical officer was called up. A few minutes later, my phone rang and the events were so typical, that I waited eagerly hoping my medical officer would make the correct diagnosis. He sounded a little unsure but at the end of the sentence he blurted out the correct diagnosis. I gave my orders and this gentleman was prepared for surgery. So much for a better health! These are some pictures to help you bloggers complete the title of this article
Case presented by Dr. G.C. George.
The answer: Perforated Gastric ulcer.

The Grand Rounds archive and schedule is available at
http://www.radiologygrandrounds.blogspot.com/
and maintained by Dr.Sumer Sethi of Sumer's Radiology Site
http://sumerdoc.blogspot.com
(quoted from http://www.filmjacket.com/news.php?readmore=54 with permission)
The most important thing is to escape responsibility or at least spread it among as many people as possible, so that you are never solely responsible for a suboptimal outcome. Here are 10 ways to do it.
Disclaimer: Of course, everything in this article is for entertainment purposes only; you should use sound medical judgment, reliable information sources and practice guidelines accepted at your institution at all times, and do everything in the best interest of patient care.
1. Request additional and/or short-term follow-up studies - if you don't know what the heck you are looking at, this may result in someone else having to read the additional/follow-up studies and carry a part of the burden of final decision.
2. Talk to the referring clinician - they may point you in the right direction and even give you the differential diagnosis. Armed with a decent differential, you may be able to produce a reasonable report.
3. Suggest clinical correlation. This is self-explanatory.
4. Call and wake up your attending - it's better to annoy them now than surprise them the next day. If your attending tells you to buzz off and hangs up on you, you've done your part - the responsibility has been spread.
You can read the rest of this piece at: http://www.filmjacket.com/news.php?readmore=54


Dr. Sumer Sethi and Dr. Joe Antony invite case submissions for the next radiology grand rounds IX on cochinblogs. The cases and/ or articles related to radiology will be put on 25th Feb 2007. Anybody interested in radiology including sonography,
conventional radiology, CT scan, MRI etc. may submit their articles, cases etc. to drjoea@gmail.com .
Here is an interesting case.
A 32 yr old comes with history of non specific pain in the knee joint.
Clinically he is normal.
MRI shows a well defined a focal altered signal intensity lesion seen in close proximity to Post cruciate ligament . It is to be differentiated from PCL tear.
Diagnosis: Posterior cruciate ligament ganglion.
Brief description of Posterior cruciate ligament
· Prevents post displacement of tibia on femur
· Extends from med femoral condyle to post and inf to tibial articular surface
· Average length 38 mm and width midpart 13 mm
· Like ACL is intraarticular and extrasynovial
· Vascular supply from middle genicular artery of popliteal vessel
· Ganglion may attach to PCL
· It is differentiated from PCL tear by demonstrating intact underlying PCL and well defined nature of ganglion.
Case presented by Dr. MGK Murthy.
Dont forget to visit our sister site: the free gallery of ultrasound images
Here you'll find loads of interesting sonographic images with a brief description and the best reference links.
A hole in the ….? A case by Dr. G.C. George (http://med97um.net/george/ )

Many have heard of a hole in the heart but for this 58 year old gentleman, it was a totally different story. He was assisted into ER, wailing in pain with every single movement. It was all too sudden. Even taking a deep breath was difficult as the pain was excruciating. He was sweating, his pulse racing, he could barely speak because the slightest effort caused him intense pain.The pain occured suddenly, all over the abdomen causing it to be so “board -like” He could barely move. He requested to be propped up to allow him to breath easily. He never had any such pain before but recently was taking some herbal traditional medication for better health! Yeah sure! My medical officer was called up. A few minutes later, my phone rang and the events were so typical, that I waited eagerly hoping my medical officer would make the correct diagnosis. He sounded a little unsure but at the end of the sentence he blurted out the correct diagnosis. I gave my orders and this gentleman was prepared for surgery. So much for a better health! These are some pictures to help you bloggers complete the title of this article

Case presented by Dr. G.C. George.
The answer: Perforated Gastric ulcer.

The Grand Rounds archive and schedule is available at
http://www.radiologygrandrounds.blogspot.com/
and maintained by Dr.Sumer Sethi of Sumer's Radiology Site
http://sumerdoc.blogspot.com